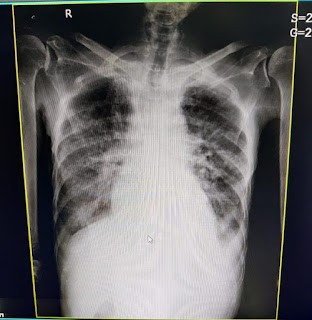
A 80 year old male patient with community acquired pneumonia
A 80 YEAR OLD MALE PATIENT PRESENTED TO OPD WITH COMPLIANTS - SHORTNESS OF BREATH AND COUGH
This is online E log book to discuss our patient’s de-identified health data shared after taking his/her/guardian’s signed informed consent. Here we discuss our individual patient’s problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs. This e-log book also reflects my patient centered online learning eportfolio and your valuable inputs on comment box is welcome .
A 80 year old male patient present to OPD with cheif complaints of shortness of breath and cough since 4 days.
HISTORY OF PRESENT ILLNESS
Patient was apparently asymptomatic 4 years back . And then he had chest pain which was radiating to the left arm for which he went to the hospital and after investigations as ecg findings show anterior wall myocardial infraction and right bundle branch block for which he underwent percutaneous transluminal coronary angioplasty in 2017. And was under medications T.ecospirin AV (70/20 )PO/OD and T.met -XL 25 mg.since then he routine life was normal.
Then he complained of lost of appetite and weight loss since 4 months and generalized weakness since 3months. H/o low backache since 3 months . Burning micturition since 3 months with frequency of 10-15 times in the night .Since 4 days he developed shortness of breath which is initially of grade 3 and progressed to grade 4 since last night associated with orthopnea and cough associated with sputum since 4 days and chills and rigors are present. Blood tinged sputum since admission. And pedal edema since 1week which is non pitting type.
No chest pain , sweating , syncopal attack , palpitations , Giddiness.
HISTORY OF PAST ILLNESS
There is History of similar complaints
History of cataract surgery B/L 6 months back
History of coronary artery disease in 2017 underwent PTCA .
PERSONAL HISTORY
Patient is vegetarian
Appetite - lost
Bowel and bladder movements - irregular
Micturition- abnormal
He was alcoholic from 25 years 90ml daily and stopped after undergoing PTCA.
He had habit of smoking since 25 years and stopped after PTCA.
GENERAL EXAMINATION
Patient is conscious , coherent , cooperative
No fever spikes since admission
Pallor present
No icterus , cyanosis, clubbing, lymphadenopathy.
Pedal edema is present and it is non pitting type
Vitals :
Temperature- afebrile
Pulse rate- 102bpm
Respiratory rate- 30cpm
Bp- 180/100mmHg
GRBS- 250mg/ dl
SYSTEMIC EXAMINATION
CVS-
Inspection- chest wall is bilaterally symmetrical
No precordial bulge
No visible pulsations , engorged veins , scars ,sinuses.
Palpation- JVP is not seen
Auscultation- S1 ,S2 heard , no murmurs
RESPIRATORY EXAMINATION- position of trachea is normal , bilateral air entry + , bilateral diffuse crepts heard in all areas .
PER ABDOMEN- soft and non- tender
CNS- patient is conscious
Speech is present
Reflexes are normal
PROVISIONAL DAIGNOSIS
Community acquired pneumonia with cystitis with denovo DM2 with benign prostatic hyperplasia with CAD S/P PTCA.
INVESTIGATIONS
HEMOGRAM
Hb- 10.9%gm/dl
TLC- 12,100cells/ cumm
Neutrophils- 84%
Lymphocytes- 8%
Esonophils- 2%
Monocytes- 6%
Basophils-0%
RBC- 3.69million/ cumm
Platelet count - 2.20lakhs/ cu.mm
LIVER FUNCTION TEST:
Total bilirubin- 1.65mg/dl
Direct bilirubin- 0.46mg/dl
AST- 89IU/L
ALT- 15IU/L
Alkaline phosphatase- 890IU/L
Total proteins- 6.5gm/dl
ALBUMIN- 3.4gm/dl
RENAL FUNCTION TEST:
Creatinine- 0.7mg/dl
Urea- 23mg/dl
Ca+2 - 9.4mg/dl
UA- 2.7mg/dl
Phosphorus- 3.1mg/dl
Na+ : 132mEq/l
K+ :3.3mEq/l
Cl- : 86mEq/l
ABG:
Ph:7.40
PCO2 :24.7mmHg
PO2: 64.5mmHg
HCO3- : 17.9mmol/l
CHCO3 : 15.2mmol/l
LIPID PROFILE:
Cholesterol- 153mg/dl
HDL-36mg/dl
LDL-99mg/dl
VLDL- 11mg/dl
20/12/21
Inj- Augmentin 1.2gm IV/ BD
Tab. Nicardia 20mg PO/ stat
Tab. Lasix 40mg PO/BD
Tab. Ecospirin AV (75/20) PO/DO
Tab. Met- XL 25mg PO/OD
Syrup - Ascoril -D 15ml PO/TID
NEB with budecort - 12th hourly , ipravent and Duolingo -6th hourly.
Inj- actrapid s/c acc to sliding scale
BIPAP INTERMITTENTLY
BP monitoring 2nd hourly
Tab.Azithromycin- 500mg PO/OD
Inj. Hydrocortisone 100mg
Inj . Deriphyline 2cc IV /stat
Inj . Tramadol 100ml NSIV / OD.
Day 2
S - cough with sputum production , cold, sob decreased a bit compared to day 1 , one fever spike present .
O- patient is conscious, coherent, oriented to time place and person.
Temp- 99°f
Pulse rate-96bpm
Respiratory rate-22cpm
Bp- 120/70mmHg
SpO2 - 96% with 10lits of O2
Grbs- 111mg/dl
Respiratory examination- bilateral air entry+, B/l inspiratory crepts + at scapular , infrascapular region.
Cvs- s1s2 +
PA - soft , contender, bowel sounds heard
Cns- no focal neurological defecit.
A- community acquired pneumonia , pulmonary kochs, h/o coronary artery disease ( post PTCA 2017), denove DM2, grade 1 prostomegaly.
P- to collect sputum ang report
-Inj AUGMENTIN 1.2 gm iv bd
Tab azithromycin 500mg po od
Neb with ipravent 6th hourly , Budecort 8th hourly , mucomist 8th hourly.
Syrup ASCORYL 10ml po tid
Tab ecospirin av (75/20) po hs
Tab metxl 25mg po.od
-Inj hai SC tid
-ivf 1NS 1RL 50ml/hr













Comments
Post a Comment