Case 8
A 55 YEAR OLD MALE PRESENTED TO OPD WITH COMPLAINTS - PEDAL EDEMA, FACIAL PUFFINESS AND SHORTNESS OF BREATH
This is online E log book to discuss our patient’s de-identified health data shared after taking his/her/guardian’s signed informed consent. Here we discuss our individual patient’s problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs. This e-log book also reflects my patient centered online learning eportfolio and your valuable inputs on comment box is welcome .
A 55 year old male who is granite cutter by occupation presented to OPD with chief complaints of swelling of both legs and face and shortness of breath and also cough.
HISTORY OF PRESENT ILLNESS
Patient was apparent asymptomatic 3months back and he developed cough which is on and off and occasionally wet cough. And 2 months back he developed pedal edema and fever which was decreased on medication and again increased this is continued for about 10days and after 2-3 days he developed shortness of breath and after about 1 week he developed facilal puffiness.
Shortness breath is aggravated by doing work and relieved by taking rest.
HISTORY OF PAST ILLNESS
He had traumatic injury to right side of his eye with stone while working.
There is no h/o of diabetes mellitus , hypertension.
PERSONAL HISTORY
Diet is mixed
Appetite is reduced
Bowel movements are irregular
He is alcoholic since 30 years and stoped 10 days back and smoking since 30 years daily 1 pack.
GENERAL EXAMINATION
Patient is concious, coherent, cooperative
Pallor is present
No cyanosis , icterus , lymphadenopathy
Bilateral pedal edema is present which is non pitting type.
Vitals :
Temperature- afebrile
Pulse rate -70bpm
Respiratory rate-20cpm
Blood pressure-140/70mmHg
SPO2- 99%
Systemic examination
CVS- S1 and S2 heard , no murmurs, no added sounds.
Respiratory system- bilateral air entry +
Trachea is in central position.
Per abdomen- soft, non tender, bowel sounds heard.
CNS- patient is concious
Speech is Present
Reflexes are normal.
PROVISIONAL DAIGNOSIS
CRF
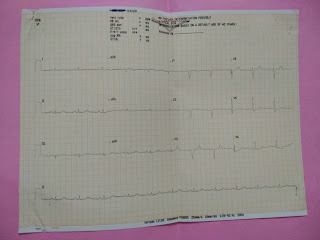
Investigation




























Comments
Post a Comment